New York Times Highlights Need to Improve Medicare Advantage
A recent investigation published in The New York Times highlights the need for Medicare Advantage (MA) improvements by calling attention to widespread allegations of fraud on the part of major private insurers participating in the program. The article, "'The Cash Monster Was Insatiable': How Insurers Exploited Medicare for Billions," examines flaws in the program's design that have led to both fraud and large, expensive plan overpayments that cost the federal government hundreds of billions of dollars and translate to higher premiums for Medicare beneficiaries.
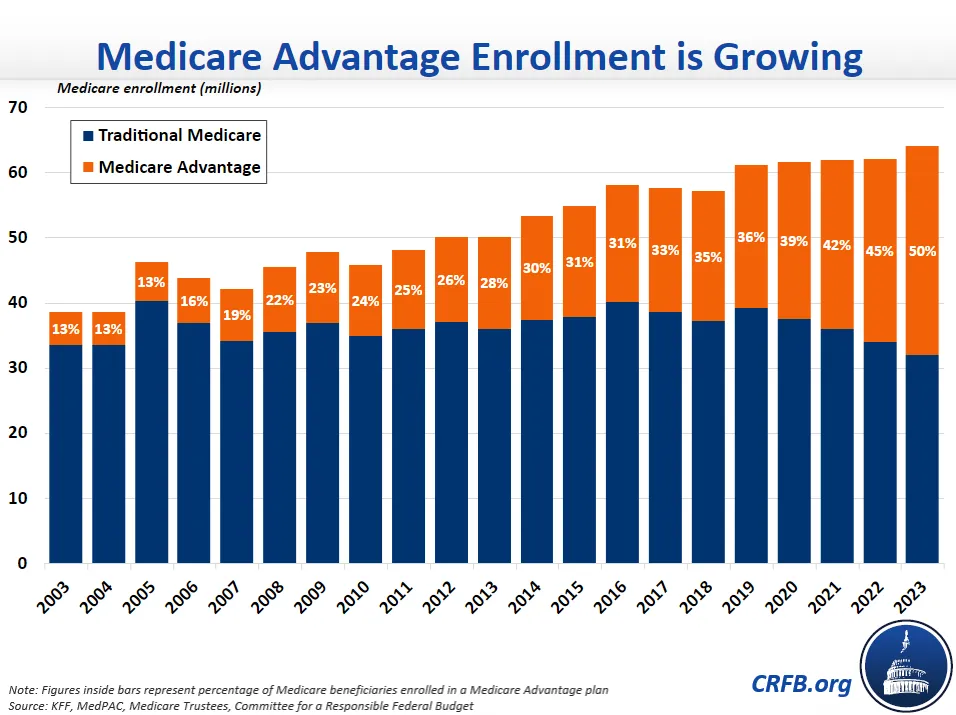
As the article points out, over half of all Medicare beneficiaries will likely be enrolled in MA by next year and over 60 percent by 2032. Since Medicare spending is higher per capita for MA enrollees than for those in traditional "fee-for-service" Medicare, this trend will result in higher federal spending on health care and a worsened outlook for the Medicare trust fund.
Part of the reason MA spends more per enrollee than traditional Medicare comes down to the way its risk adjustment system works. Payments are made based on patient diagnoses, which means providers get paid more for each additional condition being treated. This creates an incentive for doctors, nurses, and third-party contractors to record – or "code" – additional diagnoses either during patient visits or even long after through medical chart reviews, sometimes resulting in fraudulently higher payments.
According to MedPAC, these additional diagnoses resulted in $12 billion in overpayments in 2020 alone. In an analysis by our Health Savers Initiative, we found that correcting for such overpayments could save anywhere from $200 to $370 billion over ten years.
As The New York Times explains, while the Centers for Medicare and Medicaid Services (CMS) has the power to make reductions in payments for plans that over-bill, it has not yet done so. CMS also has the power to reduce payments across the board to fully correct for diagnostic coding intensity, but it has likewise never exercised this authority. In fact, CMS has continually increased MA payments. Despite clear cases of overpayment, payments are set to increase by 8.5 percent in 2023 to reflect higher inflation.
CMS recently published a request for information on how to improve the MA program, to which the Committee for a Responsible Federal Budget responded with proposals to address coding intensity and move to budget neutrality for the MA quality bonus system. While fraud is a significant issue CMS must work to address, overpayments have created a system where MA is highly profitable for private insurance companies, rather than one that saves taxpayer money by promoting more efficient forms of care.
The findings published by The New York Times serve as further evidence that, as the Medicare trust fund approaches insolvency in 2028, policymakers should consider comprehensive policies to improve MA and lower health care costs.
*****
Learn more about the status of Medicare Advantage and federal costs by checking out our in-depth analyses:
- Legislation to Bring Transparency to MA Introduced
- New MA Bill Would Increase Medicare Costs
- Committee Sends Letter to CMS on Medicare Advantage
- Analysis of the 2022 Medicare Trustees' Report
- Medicare Advantage Costs Continue to Rise
- Can Medicare Advantage Reforms Save the Trust Fund?
- Reducing Medicare Advantage Overpayments

