Is Wyden-Isakson the Future of Medicare?
Senator Johnny Isakson (R-GA) and the presumptive incoming Chairman of the Senate Finance Committee, Ron Wyden (D-OR), have sponsored a new bill that attempts to improve the way Medicare manages care for patients with chronic conditions. Although it is unclear whether the legislation will be scored as achieving any savings, it puts forward the framework for an alternative delivery system and payment model that offers the potential of providing more cost effective care and ultimately achieving savings for beneficiaries and the Medicare program.
With the 68 percent of Medicare enrollees suffering from two or more chronic conditions accounting for 93 percent of Medicare spending, and patients with at least one chronic condition accounting for 84 percent of total national health care expenditures (and 50 percent of the population), addressing the needs of these patients and better coordinating their care (which is often fragmented today) should be a critical priority of our health care system.

Source: Bipartisan Policy Center
The Wyden-Isakson proposal (also co-sponsored in the House by Reps. Peter Welch (D-VT) and Erik Paulsen (R-MN)) seeks to remedy this by creating a new option for Medicare beneficiaries – Better Care Plans (BCPs). BCPs share many traits in common with the enhanced Accountable Care Organizations (ACOs) at the heart of recent proposals from the Bipartisan Policy Center, the Brookings Institute, and Jim Capretta.
Unlike today’s ACOs, BCPs would require patients to actively enroll in a plan, which should help to engage enrollees, rather than the current model of attributing Medicare beneficiaries to ACOs administratively based on their care patterns. Health care providers who form BCPs would be given a single payment for their collective efforts to meet the health needs of qualified beneficiaries, and would be given greater tools and incentives to coordinate care and encourage more cost effective care.
BCPs would be given some flexibility to design a benefit package that would better encourage the use of high-value services through lower cost sharing requirements. However, the option for value-based insurance design would be limited to incentives for high quality care and would not allow BCPs to increase cost sharing requirements for non-BCP providers or low value services above the current Medicare cost-sharing requirements.
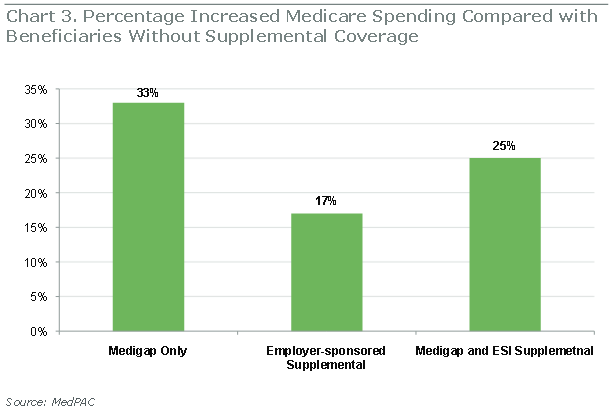
The proposal also prevents supplemental Medigap policies from covering patient cost-sharing for non-emergency services from providers not part of the BCP, to reinforce BCPs efforts to use cost-sharing requirements to direct patients to higher-value, better-suited care. Under this model, therefore, BCP enrollees who also purchase a Medigap policy would likely face strong cost-sharing incentives to receive care within their BCP.
Medigap policies, if allowed for BCP enrollees, would also undercut the effectiveness of BCPs, because of their known effects on increased utilization of care. However, it appears that employer-sponsored supplemental insurance plans, including federally-administered ones like TRICARE-for-Life, would not be prohibited from covering cost-sharing for BCP enrollees.
Source: Bipartisan Policy Center
BCPs would also be required to accept two-sided risk (sharing the burden of losses from higher spending as well as gains from lower spending) at their outset. BCPs would become available to eligible Medicare beneficiaries starting in 2017, and would further have to accept full capitation for their enrollees after three years, at the latest. To accept such risk, BCPs would have to essentially meet the insurance requirements currently required of Medicare Advantage (MA) plans (including network adequacy and financial solvency), or could simply contract with an MA plan directly. BCPs could also offer Part D (prescription drug) benefits or contract with an existing prescription drug plan to administer them.
In BCPs, state-licensed and certified providers will also be allowed to practice to the top of their license, which can help alleviate provider shortages that may exist in parts of the country. While this allowance does not preempt state licensing laws, it could help encourage states to loosen their regulations on providers’ scope of practice, and at the least removes barriers within the Medicare program.
Perhaps most distinctly, though, BCPs would only accept enrollees who have chronic condition(s). Although enrollment is limited initially, with roughly 80 percent of Medicare beneficiaries having at least one chronic condition, most of those in Medicare will become eligible eventually. If BCPs are successful in providing more effective and efficient care at a lower cost to beneficiaries as well as the Medicare program, one might even expect political and beneficiary pressure to expand BCP-eligibility to all Medicare beneficiaries at some point.
One shortcoming that may reduce the impact of the Wyden-Isakson plan is that few financial incentives are given for providers to form and beneficiaries to join a BCP. It is unclear if BCPs could offer enrollees reduced premiums, outside of if they explicitly formed as a Medicare Advantage plan. There are also no penalties or bonuses for providers who do not form or contract with a BCP. However, if BCPs were included in the existing Senate Finance SGR replacement bill as a form of Alternative Payment Model (APM), then physicians participating in a BCP could be eligible for a 5 percent bonus payment while non-APM physicians would have their payment rates frozen from 2016-2023. Notably, though, non-physician providers such as hospitals and post-acute care facilities would still face no such incentives to participate in a BCP.
Controlling the growth of Medicare spending will require us to change the way we deliver and pay for care to make the system more cost effective. Senators Wyden and Isakson and Representatives Paulsen and Welch are to be commended for putting forward a thoughtful proposal designed to shift away from volume-based reimbursement toward paying for quality and coordination of care.
Given that Senator Wyden will likely soon become the Chairman of the Senate Finance Committee, this bill may provide insight into what the Alternative Payment Models (APMs) in the SGR replacement bill might look like. BCPs are a form of enhanced ACOs in many ways, but may also co-exist with them quite well for a period of time. If this legislation or a similar proposal to improve care coordination were enacted, the basic framework of BCPs or other coordinated care models could be improved and strengthened to achieve greater savings as policymakers see how they work.
Regardless of its fate, the Wyden-Isakson proposal makes a valuable contribution to the discussion about the future of Medicare by putting forward a model that offers the potential of providing better quality care at a lower cost.